Polymyalgia Rheumatica and Coronavirus: Understanding the Intersection of Two Health Challenges
In the wake of the ongoing global pandemic caused by the novel coronavirus, medical researchers and professionals have been paying increasing attention to the interaction between COVID-19 and pre-existing medical conditions. One such condition that has gained interest is polymyalgia rheumatica (PMR), a relatively common inflammatory disorder that predominantly affects older adults. This article delves into the relationship between polymyalgia rheumatica and coronavirus, exploring how these two health challenges intersect and impact individuals.
Polymyalgia Rheumatica: A Brief Overview
Polymyalgia rheumatica is an autoimmune disorder characterized by widespread pain and stiffness in the muscles, particularly around the shoulders, hips, neck, and upper arms. While the exact cause of PMR remains unclear, it is thought to result from a combination of genetic predisposition and environmental triggers. Symptoms often develop rapidly, causing significant discomfort and reducing the affected individual's quality of life. The condition predominantly affects individuals over the age of 50 and is more common in women than men.
COVID-19 and Its Implications
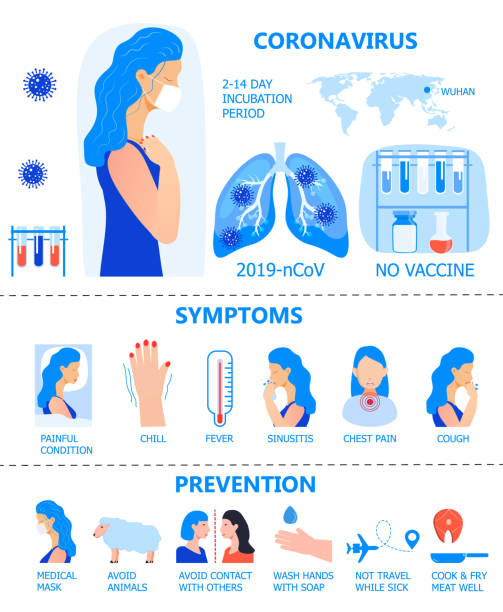
COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), primarily presents as a respiratory illness. However, as the pandemic has progressed, it has become evident that the virus can have a wide range of effects on the body beyond the respiratory system. These effects can vary from mild symptoms to severe complications, including acute respiratory distress syndrome (ARDS), cytokine storms, and multiorgan dysfunction.
Older adults and those with underlying health conditions have been identified as particularly vulnerable to severe COVID-19 outcomes. Conditions such as hypertension, diabetes, cardiovascular disease, and respiratory disorders have been highlighted as risk factors. Given that polymyalgia rheumatica predominantly affects an older demographic, it is important to consider the potential implications of COVID-19 for individuals with PMR.
The Intersection: Polymyalgia Rheumatica and COVID-19
The intersection between polymyalgia rheumatica and COVID-19 is multifaceted. Both conditions involve the immune system, and there is evidence to suggest that an overactive immune response plays a role in the severity of COVID-19 symptoms. In the case of PMR, the immune system mistakenly attacks healthy tissues, leading to inflammation and pain. This chronic inflammatory state might impact how an individual's body responds to the viral infection, potentially influencing the course of COVID-19.
Furthermore, the symptoms of polymyalgia rheumatica, such as muscle pain and stiffness, might overlap with some of the common symptoms of COVID-19, such as body aches and fatigue. This overlap can lead to diagnostic challenges, especially in cases where individuals with PMR contract the virus. Distinguishing between the two conditions becomes crucial for appropriate medical management and care.
Managing Polymyalgia Rheumatica During the Pandemic
For individuals living with polymyalgia rheumatica, the pandemic has brought unique challenges. Many patients with PMR rely on corticosteroids to manage their symptoms, as these medications help reduce inflammation and pain. However, corticosteroids can suppress the immune system, potentially making individuals more susceptible to infections, including COVID-19.
Rheumatologists and healthcare providers have had to carefully balance the benefits of managing PMR symptoms with the potential risks of immunosuppression during the pandemic. In some cases, alternative treatment strategies that minimize corticosteroid use have been explored to reduce the overall risk for these individuals.
Preventive Measures and Considerations
Individuals with polymyalgia rheumatica should adhere to preventive measures recommended by public health authorities to reduce their risk of contracting COVID-19. These measures include wearing masks, practicing physical distancing, and maintaining good hand hygiene. Additionally, staying up to date with vaccinations, including the COVID-19 vaccine, is crucial for individuals with PMR to protect themselves from severe illness.
In conclusion, the interaction between polymyalgia rheumatica and coronavirus is a complex and evolving area of study. The immune system's role in both conditions adds a layer of intricacy to how they intersect. The challenges faced by individuals with PMR during the pandemic highlight the importance of a holistic approach to healthcare, considering not only the specific condition but also its potential interactions with other health challenges. As medical understanding of both PMR and COVID-19 continues to grow, it is hoped that improved insights will lead to better management strategies for those affected by these conditions.
In the wake of the ongoing global pandemic caused by the novel coronavirus, medical researchers and professionals have been paying increasing attention to the interaction between COVID-19 and pre-existing medical conditions. One such condition that has gained interest is polymyalgia rheumatica (PMR), a relatively common inflammatory disorder that predominantly affects older adults. This article delves into the relationship between polymyalgia rheumatica and coronavirus, exploring how these two health challenges intersect and impact individuals.
Polymyalgia Rheumatica: A Brief Overview
Polymyalgia rheumatica is an autoimmune disorder characterized by widespread pain and stiffness in the muscles, particularly around the shoulders, hips, neck, and upper arms. While the exact cause of PMR remains unclear, it is thought to result from a combination of genetic predisposition and environmental triggers. Symptoms often develop rapidly, causing significant discomfort and reducing the affected individual's quality of life. The condition predominantly affects individuals over the age of 50 and is more common in women than men.
COVID-19 and Its Implications
COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), primarily presents as a respiratory illness. However, as the pandemic has progressed, it has become evident that the virus can have a wide range of effects on the body beyond the respiratory system. These effects can vary from mild symptoms to severe complications, including acute respiratory distress syndrome (ARDS), cytokine storms, and multiorgan dysfunction.
Older adults and those with underlying health conditions have been identified as particularly vulnerable to severe COVID-19 outcomes. Conditions such as hypertension, diabetes, cardiovascular disease, and respiratory disorders have been highlighted as risk factors. Given that polymyalgia rheumatica predominantly affects an older demographic, it is important to consider the potential implications of COVID-19 for individuals with PMR.
The Intersection: Polymyalgia Rheumatica and COVID-19
The intersection between polymyalgia rheumatica and COVID-19 is multifaceted. Both conditions involve the immune system, and there is evidence to suggest that an overactive immune response plays a role in the severity of COVID-19 symptoms. In the case of PMR, the immune system mistakenly attacks healthy tissues, leading to inflammation and pain. This chronic inflammatory state might impact how an individual's body responds to the viral infection, potentially influencing the course of COVID-19.
Furthermore, the symptoms of polymyalgia rheumatica, such as muscle pain and stiffness, might overlap with some of the common symptoms of COVID-19, such as body aches and fatigue. This overlap can lead to diagnostic challenges, especially in cases where individuals with PMR contract the virus. Distinguishing between the two conditions becomes crucial for appropriate medical management and care.
Managing Polymyalgia Rheumatica During the Pandemic
For individuals living with polymyalgia rheumatica, the pandemic has brought unique challenges. Many patients with PMR rely on corticosteroids to manage their symptoms, as these medications help reduce inflammation and pain. However, corticosteroids can suppress the immune system, potentially making individuals more susceptible to infections, including COVID-19.
Rheumatologists and healthcare providers have had to carefully balance the benefits of managing PMR symptoms with the potential risks of immunosuppression during the pandemic. In some cases, alternative treatment strategies that minimize corticosteroid use have been explored to reduce the overall risk for these individuals.
Preventive Measures and Considerations
Individuals with polymyalgia rheumatica should adhere to preventive measures recommended by public health authorities to reduce their risk of contracting COVID-19. These measures include wearing masks, practicing physical distancing, and maintaining good hand hygiene. Additionally, staying up to date with vaccinations, including the COVID-19 vaccine, is crucial for individuals with PMR to protect themselves from severe illness.
In conclusion, the interaction between polymyalgia rheumatica and coronavirus is a complex and evolving area of study. The immune system's role in both conditions adds a layer of intricacy to how they intersect. The challenges faced by individuals with PMR during the pandemic highlight the importance of a holistic approach to healthcare, considering not only the specific condition but also its potential interactions with other health challenges. As medical understanding of both PMR and COVID-19 continues to grow, it is hoped that improved insights will lead to better management strategies for those affected by these conditions.